Introduction: disease prevention as the most important public service
The COVID-19 pandemic has indelibly shown the importance of disease prevention as a fundamental public service. Whilst we spend over ten per cent of GDP on healthcare1, the focus is on expensive late-stage health interventions that address the consequences but not the origins of poor health: indeed 99% of the government’s health expenditure funds the treatment rather than the prevention of ill health2. Obesity alone costs the NHS £6 billion annually3; and a staggering 80% of non-communicable diseases such as heart disease, diabetes and cancer are thought to be preventable4. The UK is becoming less healthy, with life expectancy falling to its lowest level in a decade5. Economic inactivity amongst working age adults is increasing6 with long-term illness now the primary reason for unemployment7, and the total economic cost of lost output among working-age people due to ill health is around £150bn per annum8.
Prevention of disease should therefore command the attention of our economists and politicians as much as doctors. Our public health service can solve for these problems by using AI to power a personalised disease prevention platform.
We need to improve our approach to disease prevention
Knowing that interventions at a population level are more effective than targeting at-risk groups, public health experts have historically favoured interventions such as legislation and regulation that tackle the social and environmental causes of disease. Such measures are unpopular with the public9, however, and are often sub-optimally implemented due to fears of ‘nanny-statism’10. Indeed, 95 of the public think the responsibility for staying healthy lies with individual11. The government is aware of this tension, and last year opened an inquiry into prevention in health and social care12. The Chief Medical Officer highlighted the need to personalise prevention in their 2016 annual report13, and the government has expressed commitment to personalised prevention since 201914.
Until recently, however, we have lacked the technology that would allow us to implement effective personalised prevention programmes. Traditional approaches require extrapolation from population-level studies without taking into account heterogeneity between individuals, because the computational power has not existed to retrieve and analyse all the variables needed to deliver a personalised result. Modern techniques allow us to collect vast and ever-increasing amounts of individual-level data, uncovering for the first time the huge range of unique factors that drive each person’s risk of disease. There is now the opportunity to revolutionise how we approach our vast public health data estate, by using AI to predict and therefore to prevent illness in a much more precise and quantitative manner.
The case for using AI in disease prevention
The emergence of AI should strategically transform the way we deliver disease prevention as a public service. The public sector can use the computational power of AI to meaningfully analyse large and varied individual-level datasets of electronic health records, and then use those latent insights to deliver personalised disease prevention plans. This approach will empower citizens to have greater control over their own health, by helping them better understand their individual levels of risk and supporting them in real time to make meaningful changes to their health. It will enable optimal use of limited resources in prevention by complementing more traditional population-level model with a more targeted service for citizens.
The proposal: an AI-powered personalised disease prevention platform
Concept
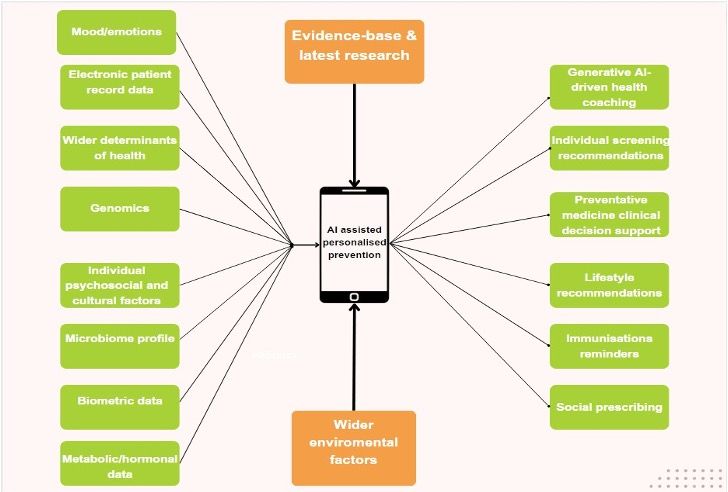
We should use AI to deliver a publicly provided platform that is predictive, prescriptive, and preventative. Such a platform could consolidate and process input from fragmented data sources: health records held by public bodies, the results of optional extra collection (genomics, psychosocial, microbiome, metabolic/hormonal, and biometric), and real-time environmental data (air pollution, communicable disease transmission statistics, and up-to-date research evidence). By unifying this data to create a single holistic view of each patient, the platform would support patient-specific health promotion and disease prevention through products such as personalised health coaching, individualised recommendations for screening and immunisations, decision support for clinicians in prescribing preventative medicines, and advice on how to access other public services.
Data sources
The UK already has rich sources of longitudinal health data that can help drive personalised prevention, but its potential is not being realised today due to fragmentation. Although launch of the Federated Data Platform is a step towards public health data integration, by linking data collected by NHS trusts and regional health systems15, AI will be able to further integrate different data sources including primary care data and social and environmental inputs that influence health, such as employment, housing, and education data.
These data can be combined with more traditional data sources such as lifestyle and biometric factors to provide a detailed picture of general health status and future disease risk. As AI is trained on this data, new digital biomarkers will emerge that will help the platform evolve constantly, becoming more precise and personalised. For example, AI has already been used in eye checks to provide cardiovascular disease screening using retinal images and could also be used to screen for other conditions such as heart failure and Parkinson’s disease16. As the data estate grows, the complete genetic and molecular characterisation, clinical course, and outcome of individuals can be used to develop a living database that can facilitate advances in prevention17. Furthermore, the cost of whole genome sequencing is continuing its sharp downwards trajectory towards affordability at a population level - with government- backed initiatives such as Our Future Health18 and the 100,000 Genomes Project19 demonstrating the huge potential of genomics. AI has the computational power to both analyse the enormity of whole genome and generate bespoke preventative recommendations to help individuals manage their personal genetic risks.
Advances in technology mean that wearable devices can now collect information tracking physiology, activity, and biochemical molecules – for example, sleep patterns, blood pressure, electrocardiography (to precent arrythmias and coronary heart disease), blood sugar, and risk of falls. The platform can accordingly deploy AI to help individuals understand how best to engage in healthy behaviours to stop disease developing in the first instance. For those with chronic health conditions, AI can remotely monitor early signs of deterioration and prevent deterioration. Allowing both patients and clinicians to proactively monitor disease status could have dramatic effects on personal health outcomes and systemic use of, and cost to, our public health services.
AI-driven preventative interventions
This strategy can drive patients’ greater ownership of their health, reducing the information asymmetry between doctor and patient. Individual engagement and involvement in health is a huge differentiator between poor and good health outcomes. There is research that shows 60% of a patient’s healthcare outcomes are driven by their behaviour and only 10% by their clinical care (with the remaining 30% driven by genetics)20.
In traditional healthcare delivery, preventative interventions are limited to a handful of touchpoints with clinicians, with the patient responsible for maintaining motivation independently in the interim. However, an AI- driven virtual health assistant (for example, GPT-4 which can mimic human-like speech and reasoning) could understand natural language and answer medical questions from patients, offer customised health recommendations and support with, for example, difficult behavioural change or medication concordance, where our existing model leaves patients comparatively unsupported.
Indeed, our health service can use behavioural science tools to understand how to drive sustainable lifestyle changes over the long term. To date, virtual medical assistant solutions have existed only in the private market—for example, the wide range of personal medical AI at varying stages of development for the management and potential reversal of diabetes through monitoring and coaching21. The WHO, however, has recently developed a virtual health assistant to help fight misinformation and support healthier behaviours22, and there is huge potential to positively transform preventative healthcare by making virtual health monitoring and coaching available as a public service, rather than only to those private citizens who can afford it.
AI will also be able to identify which preventative activities are appropriate for individuals, whose healthcare plan will no longer then be determined at a macro level. Screening, for instance, is one of the major preventative public services but the current model is based on traditional population- level public health methodology. This approach requires the participation of huge numbers of people, some of whom will undergo unnecessary procedures, or biopsies, to identify disease in very few. Although mass screening is effective at a population level, it is known that at an individual level it can lead to overdiagnosis, unnecessary treatment or false reassurance23 24 25. There is potential to use AI to radically disrupt the current approach. An AI-driven platform which takes account of each patient’s specific risk factors to deliver an individualised screening plan based on risk profile will result in a safer, more efficient, and less costly screening service.
Implementation
The UK is perfectly positioned to be the world leader in the use of AI to revolutionise its approach to disease prevention. We have the academic capital, a national healthcare system with a cohesive and robust approach to data collection, and a genuine need to invest heavily in disease prevention to support the publicly-funded NHS. The platform can be implemented in relatively short order, and then iterate as new research and technology develop.
A suggested roadmap of immediate steps could comprise:
Creation of a cross-government working group on personalised prevention bringing together stakeholders from inter alia NHS England, DHSC, devolved governments, UKHSA, Genomics England, and Our Future Health.
Formation of an “AI in Healthcare Ethics Council”, consisting of experts from medicine, ethics, genomics and technology including those from the Nuffield Council on Bioethics and Ada Lovelace Institute, who are currently leading thinking on the ethics of AI and genomics26. This independent steering group would oversee the ethical and equitable deployment of the platform, and provide accountability to ensure transparency. This would support public engagement and trust in the project.
Development of the secure data architecture needed to underpin an AI-driven personalised prevention platform, including mechanisms for safeguarding patient privacy and addressing systemic biases in data and algorithms.
Conclusion
At a societal level, our most fundamental public service is surely disease prevention. We can now use the power of AI to transform our approach to this, and thereby to transform the health of our population. There is significant executive need for this project: the UK Government has stated that it aims for the UK to be “the most advanced genomic healthcare system in the world”27, has positioned the UK as a “global superpower in AI”28, and in its recent Major Conditions Strategy articulated an ambitious framework to reduce the burden of chronic disease including a commitment to personalised prevention29.
There is also pressing social demand: the huge success of the NHS App30 demonstrates public appetite for the democratisation of medical knowledge delivered via digital means. By building an integrative disease prevention platform, we can use AI to make citizens active participants in their own preventative healthcare before they are sick and require costly reactive treatment; and embed their investment in their own health, in real time, in a way that is truly personal and accessible to them. Users of our public health service are becoming sicker31 but they are also inhabitants of the Fourth Industrial Revolution. How can public services better improved than by using AI to provide users with a personalised means of disease prevention before a cure is needed?
References
- Prendergast, T. (2023). Healthcare expenditure, UK Health Accounts provisional estimates - Office for National Statistics. [online] www.ons.gov.uk. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare
/healthcaresystem/bulletins/healthcareexpendit
ureukhealthaccountsprovisionalestimates/2022. [Accessed 16 Dec. 2023]. - Tony Blair Institute for Global Change (2023). Fit for the Future: How a Healthy Population Will Unlock a Stronger Britain. [online] Available at: https://www.institute.global/insights/public-services/fit-future-how-healthy-population-will- unlock-stronger-britain#footnote_list_item_17 [Accessed 16 Dec. 2023].
- Department of Health and Social Care (2022). New obesity treatments and technology to save the NHS billions. [online] GOV.UK. Available at: https://www.gov.uk/government/news/new-obesity-treatments-and-technology-to-save-the-nhs- billions. [Accessed 16 Dec. 2023].
- NCD Alliance. (2015). NCDs. [online] Available at: https://ncdalliance.org/why- ncds/NCDs#:~:text=An%20estimated%2080%25%20of%20NCDs. [Accessed 16 Dec. 2023].
- Buxton, J. (2024). National life tables – life expectancy in the UK - Office for National Statistics. [online] www.ons.gov.uk. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/
birthsdeathsandmarriages/lifeexpectancies/bulletins/
nationallifetablesunitedkingdom/2020to2022. [Accessed 16 Dec. 2023]. - Watson, B. (2023). A05 SA: Employment, unemployment and economic inactivity by age group (seasonally adjusted) - Office for National Statistics. [online] Available at: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork
/employmentandemployeetypes/datasets/employmentun employmentandeconomicinactivitybyagegroupseasonallyadjusteda05sa [Accessed 15 Dec. 2023]. - Watson, B. (2023b). INAC01 SA: Economic inactivity by reason (seasonally adjusted) - Office for National Statistics. [online] Available at: https://www.ons.gov.uk/employmentandlabourmarket/peoplenotinwork
/economicinactivity/datasets/economicinactivitybyre asonseasonallyadjustedinac01sa. [Accessed 16 Dec. 2023]. - Robert, C. (2023). The economic cost of ill health among the working-age population. [online] Oxera. Available at: https://www.oxera.com/insights/reports/the-economic-cost-of-ill-health-among-the-working-age-population/ [Accessed 16 Dec. 2023].
- Snowdon, C. (2017). Killjoys: A Critique of Paternalism. London Publishing Partnership.
- Mahase, E. (2023). Obesity: Politicians’ fears over ‘nanny-statism’ have contributed to failed strategies, says report. BMJ, 381, p.900. doi:https://doi.org/10.1136/bmj.p900.
- Health Foundation (2023). Public perceptions of health and social care (November 2022) - The Health Foundation. [online] www.health.org.uk. Available at: http://health.org.uk/publications/public-perceptions-of-health-and-social-care- november-2022 [Accessed 26 Jan. 2024].
- UK Parliament (2023). Prevention in health and social care. [online] Available at: https://committees.parliament.uk/work/7205/prevention-in-health-and-social-care/news/ [Accessed 17 Dec. 2023].
- Davies, S. (2016). Chief Medical Officer annual report 2016: generation genome. [online] GOV.UK. Available at: https://www.gov.uk/government/publications/chief-medical-officer-annual-report-2016-generation-genome. [Accessed 17 Dec. 2023].
- Department of Health and Social Care (2019). Advancing our health: prevention in the 2020s – consultation document. [online] GOV.UK. Available at: https://www.gov.uk/government/consultations/advancing-our-health-prevention-in-the- 2020s/advancing-our-health-prevention-in-the-2020s-consultation-document. [Accessed 26 Jan. 2024]
- NHS England (2023). NHS England: Federated Data Platform update. [online] www.england.nhs.uk. Available at: https://www.england.nhs.uk/long-read/federated-data-platform-update/ [Accessed 17 Dec. 2023].
- Zhou, Y., Chia, M.A., Wagner, S.K., Ayhan, M.S., Williamson, D.J., Struyven, R.R., Liu, T., Xu, M., Lozano, M.G., Woodward-Court, P., Kihara, Y., Altmann, A., Lee, A.Y., Topol, E.J., Denniston, A.K., Alexander, D.C. and Keane, P.A. (2023). A foundation model for generalizable disease detection from retinal images. Nature, [online] 622, pp.156–163. doi:https://doi.org/10.1038/s41586-023-06555-x.
- Snyder, M. P. (2016). Genomics and personalized medicine : what everyone needs to know. New York Oxford University Press, p.128.
- Our Future Health. (2022). How Our Future Health works. [online] Available at: https://ourfuturehealth.org.uk/our- research-mission/how-our-future-health-works/ [Accessed 18 Dec. 2023].
- Genomics England (2022). 100,000 Genomes Project. [online] Genomics England. Available at: https://www.genomicsengland.co.uk/initiatives/100000-genomes-project. [Accessed 7 Jan. 2024].
- Schroeder, S.A. (2007) We Can Do Better—Improving the Health of the American People. New England Journal of Medicine, 12, 1221-1228. https://doi.org/10.1056/NEJMsa073350
- Topol, E.J. (2019). Deep Medicine : How Artificial Intelligence Can Make Healthcare Human Again. New York: Basic Books, March, p.263.
- WHO (2022). Using AI to lead a healthier lifestyle | World Health Organization. [online] www.who.int. Available at: https://www.who.int/campaigns/Florence [Accessed 7 Jan. 2024].
- Welch, H.G. (2017). Cancer Screening, Overdiagnosis, and Regulatory Capture. JAMA Internal Medicine, 177(7), p.915. doi:https://doi.org/10.1001/jamainternmed.2017.1198.
- Welch, H.G., Prorok, P.C., O’Malley, A.J. and Kramer, B.S. (2016). Breast-Cancer Tumor Size, Overdiagnosis, and Mammography Screening Effectiveness. New England Journal of Medicine, 375(15), pp.1438–1447. doi:https://doi.org/10.1056/nejmoa1600249.
- Petticrew, M., Sowden, A. and Lister-Sharp, D. (2001). FALSE-NEGATIVE RESULTS IN SCREENING PROGRAMS. International Journal of Technology Assessment in Health Care, 17(2), pp.164–170. doi:https://doi.org/10.1017/s0266462300105021.
- Farmer, H. (2023). AI and genomics. [online] The Nuffield Council on Bioethics. Available at: https://www.nuffieldbioethics.org/publications/ai-and-genomics-futures.
- Department of Health and Social Care (2021). New implementation plan to deliver world-leading genomic healthcare. [online] GOV.UK. Available at: https://www.gov.uk/government/news/new-implementation-plan-to-deliver-world-leading- genomic-healthcare#:~:text=New%20actions%20set%20out%20today [Accessed 18 Dec. 2023].
- GOV.UK (2021). National AI Strategy. [online] GOV.UK. Available at: https://www.gov.uk/government/publications/national-ai-strategy. [Accessed 26 Jan. 2024].
- Department of Health and Social Care (2023). Major conditions strategy: case for change and our strategic framework. [online] GOV.UK. Available at: https://www.gov.uk/government/publications/major-conditions-strategy-case-for-change- and-our-strategic-framework/major-conditions-strategy-case-for-change-and-our-strategic-framework--2#chapter-2-keeping- people-healthy-through-primary-and-secondary-prevention. [Accessed 26 Jan. 2024].
- NHS England (2023). NHS England» NHS App reaches record users on fifth anniversary. [online] www.england.nhs.uk. Available at: https://www.england.nhs.uk/2023/12/nhs-app-reaches-record-users-on-fifth- anniversary/#:~:text=The%20NHS%20App%20has%20twice [Accessed 26 Jan. 2024].
- Health Foundation (2023). 2.5 million more people in England projected to be living with major illness by 2040. [online] www.health.org.uk. Available at: https://www.health.org.uk/news-and-comment/news/25-million-more-people-in-england- projected-to-be-living-with-major-illness-by-2040#:~:text=Overall%2C%20the%20number%20of%20people. [Accessed 16 Dec. 2023].